6 to 7 million people in the United States live with chronic venous insufficiency. Around 150,000 new people are diagnosed every year(1).
Chances are that someone you know has this condition – or that someone may even be you!
Chronic venous insufficiency may be known for its symptoms: leg swelling, skin changes, and discomfort. But chronic venous insufficiency can be a sign of something worse down the road. It’s important to familiarize yourself with this condition.
Let’s learn how to identify chronic venous insufficiency: the causes, signs, symptoms, and treatment options.
Table of Contents
ToggleHow does chronic venous insufficiency start?
Chronic venous insufficiency is classified as either primary or secondary:
Patients with primary chronic venous insufficiency may be born with the condition. They might have abnormal vein walls or less elastin, which means their veins don’t stretch as well as others. In any case, these issues are out of one’s control and do not stem from another condition.
Secondary chronic venous insufficiency is, well, secondary to another condition. And it often develops because the patient already has deep vein thrombosis.
Deep vein thrombosis, or DVT, is a disease where blood clots form in the veins, usually in the legs(3). DVT triggers inflammation, causing damage to vein walls. This causes secondary chronic venous insufficiency.
Someone may have an increased risk of developing CVI if they are female, obese, or pregnant. Smoking also increases risk. Prolonged standing and having May-Thurner syndrome do as well(1).
The veins bring blood back to the heart, pushing blood upwards from the legs. To do this, the muscles of the calves and the valves of the veins work together.
However, chronic venous insufficiency patients may experience leaks or obstruction in the veins. This results in a pressure increase in the lower extremities. Blood flow, vein blockages, valves, and calf muscles all impact pressure.
When CVI is secondary to DVT, repeated vein wall injury from DVT causes the veins to scar. These scars narrow the blood passageway, increasing venous pressure.
Chronic Venous Insufficiency Symptoms
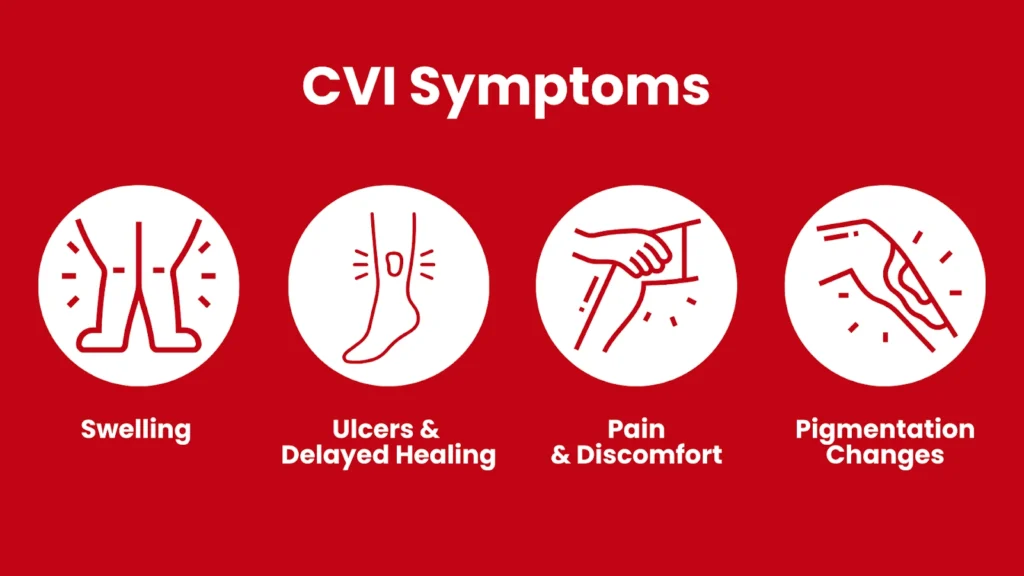
Patients with CVI experience pain, leg discomfort, ankle and leg swelling, or itching. They may also feel “prickling,” cramping, or heaviness in the lower limbs after standing too long(4).
In severe cases, ulcers, pigmentation, thickening, and wound healing delays are possible. Ulcers near the ankles may especially have trouble healing.
Diagnosis of Chronic Venous Insufficiency
To diagnose chronic venous insufficiency, the doctor might ask if:
- You’ve ever been pregnant
- You have a family history of CVI
- Your job job involves heavy lifting or prolonged standing
They will also review your full medical history. They’ll look for conditions like obesity and hypertension. The doctor will also examine your legs, noting size, texture, and color.
The doctor may also test for D-dimer levels. This is a protein released as blood clots form. Levels may be higher in patients with CVI(5).
If they suspect CVI, you might receive more testing. One example is the venous duplex ultrasound scan. This is one of the best way to locate problematic veins(6)
Venous plethysmography is another noninvasive test. This uses infrared light to determine the amount of blood pumped during exercise. The physician can measure the amount of leakage, obstruction, or muscle use.
Your physician might request magnetic resonance venography. This test is much more invasive and only for complex CVI cases(7).
Your doctor may also rule out other conditions with MRI or CT scans.
Chronic Venous Insufficiency Classification
Clinical, Etiology, Anatomic, and Pathophysiology (CEAP) classification helps physicians consistently identify and treat vein disease(8):
- Clinical (C) classification divides vein disease into categories of severity based on symptoms.
- Etiologic (E) helps describe the disease’s cause.
- Anatomic (A) identifies which veins are insufficient.
- Pathophysiological (P) helps identify how the disease impacts the body. (Examples include reflux, thrombosis, or obstruction.)
Doctors also classify CVI with Venous Clinical Severity Scoring, or VCSS. VCSS uses different attributes to identify disease severity: absent, mild, moderate, or severe. This is often used in assessing the patient’s response to treatment(8).
Table 1.CEAP Classification. (8)
Chronic Venous Insufficiency Treatments
CEAP classification and VCSS will identify CVI severity. From there, the doctor will recommend treatment.
The goal of treatment is to improve circulation and prevent further vein damage. Treatments might also focus on reducing swelling, healing venous ulcers, and managing pain.
Treatments include:
Lifestyle changes
Smoking causes several health problems, including vein issues. Smoking restricts the blood flow in our lower limbs. Nicotine also impacts vein elasticity. Stopping a smoking habit can greatly improve your vein health.
Eating a balanced diet is also crucial. Extra weight on your body can add extra stress on your legs, worsening symptoms.
Blood flow improvements
Elevating your legs can help improve blood flow. Try sitting with the legs raised above the thighs or lying down with the legs above your heart. This also reduces leg swelling.
Another way to improve blood flow is to do regular exercises. Rehabilitation through exercise is also available. CVI patients saw improvements in 5 months after regular calf muscle exercise(10).
Compression stockings are a standard treatment for helping to restore venous blood flow. Compression is greatest around the ankle. This pressure decreases as you move up the leg, aiding blood flow(9).
Medications
The US Food and Drug Administration has not approved any medications for CVI. Medications may be prescribed to treat side effects.
Your doctor may prescribe diuretics to reduce leg swelling. Horse chestnut seed extracts, French maritime pine bark extract, and flavonoids can also help(2).
Venoablation
Venoablation is a surgical treatment for severe chronic venous insufficiency. Venoablation removes veins that serve as reflux pathways(9). Removing these veins may help with ulcer healing and symptom improvement.
Sclerotherapy is one type of venoablation. The physician inserts a substance into a specific vein. This substance destroys the vein. This is often used in smaller widened veins rather than CVI.
Radiofrequency ablation, or RFA, is another technique. The doctor uses radio waves to produce an electrical current that heats the vein, closing it off(9).
Less than 8% of CVI patients require venoablation as it depends on the patient’s condition.
Patients with severe symptoms are often treated with vein ligation with stripping. The doctor will perform ultrasound mapping beforehand to ensure patient safety(11).
Chronic Venous Insufficiency Complications
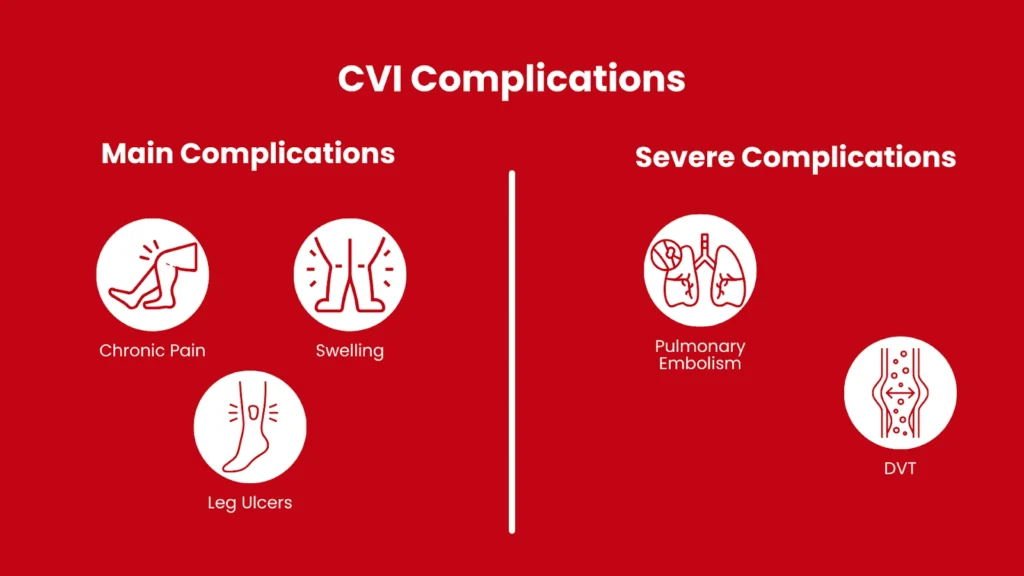
The most common CVI complications include:
- Chronic leg pain
- Swelling
- Non-healing leg ulcers are the most common CVI complications.
Other less severe complications include venous ulcerations and secondary lymphedema.
It is important to treat CVI to avoid worse outcomes. Examples include deep vein thrombosis or pulmonary embolism.
A blood clot travels from the lower limbs to the lungs. This blocks the passage of blood and causes rapid body deterioration or even death.
Seek medical treatment right away if you’re experiencing a pulmonary embolism.
Conclusion
Chronic venous insufficiency is nothing to make light of. Leaving CVI untreated can lead to disability down the road.
When CVI starts, it does not stop. It is a persistent condition. Pain, skin issues, and ulceration will progress. DVT and pulmonary embolism become more possible.
Early diagnosis will save you time and money – and may even save your life.
If you’re ready to take charge of your vein health, the experts at Texas Vein Experts are ready. Our team is here to provide solutions for chronic venous insufficiency. Our vein experts are professional and patient-focused, providing top-of-the-line care and modern treatments like radiofrequency ablation and sclerotherapy.
Take the first step toward a healthier you. Book your free consultation today!
References:
- De Popas, E., & Brown, M. (2018). Varicose Veins and Lower Extremity Venous Insufficiency. Seminars in interventional radiology, 35(1), 56–61. https://doi.org/10.1055/s-0038-1636522
- Jameson, J. L., Kasper, D. L., Longo, D. L., Fauci, A. S., Hauser, S. L., &Loscalzo, J. (2018). Harrisons principles of internal medicine 20th edition. New York: McGraw-Hill Education.
- Waheed, S. M., Kudaravalli, P., &Hotwagner D. T. (2020). Deep vein thrombosis. StatPearls.Treasure Island: StatPearls Publishing
- Spiridon, M., &Corduneanu, D. (2017). Chronic Venous Insufficiency: a Frequently Underdiagnosed and Undertreated Pathology. Maedica, 12(1), 59–61.
- Bounds E. J., Sankar P., Kok S. J. (2020) D imer. StatPearls. Treasure Island: StatPearls Publishing
- Necas M. (2010). Duplex ultrasound in the assessment of lower extremity venous insufficiency. Australasian journal of ultrasound in medicine, 13(4), 37–45.
- Tamura, K., & Nakahara, H. (2014). MR Venography for the Assessment of Deep Vein Thrombosis in Lower Extremities with Varicose Veins. Annals of vascular diseases, 7(4), 399–403. https://doi.org/10.3400/avd.oa.14-00068
- Eberhardt, R. T., &Raffetto, J. D. (2014). Chronic venous insufficiency. Circulation: Clinical Summaries. 130:293–294. https://doi.org/10.1161/CIR.0000000000000083
- Weiss, R., Anariba, D. E. Z., Lanza, J., &Lessnau, K. D. (2018). Venous insufficiency. Retrieved from https://emedicine.medscape.com/article/1085412-treatment
- Kahle B, Leng K. Efficacy of sclerotherapy in varicose veins: prospective, blinded, placebo-controlled study.Dermatol Surg. 2004; 30:723–728.
- Ombrellino, M., &Kabnick, L. S. (2005). Varicose vein surgery. Seminars in interventional radiology, 22(3), 185–194. https://doi.org/10.1055/s-2005-921951




