We sometimes feel fidgety sitting in the same place for too long and may feel the urge to move our legs.
But this urge is more than that for up to one-tenth of adults. This urge can become a nuisance. They may suffer from restless legs syndrome.
Restless legs syndrome (RLS) is a chronic limb disease where patients regularly fight an urge to move their legs. RLS sufferers can have trouble sleeping with symptoms worsening at night.
This disease is often underdiagnosed, leading to a delay in treatment(1). But education is the first step toward treatment. Learn more about RLS and its causes, diagnosis, and treatment options.
Table of Contents
ToggleWhat is restless legs syndrome (RLS)?
Many people live with RLS: an estimated 7-10% of the population. Women are more likely than men to suffer from this condition(2).
The disorder starts in early childhood. However, patients usually won’t receive a diagnosis until their 30s*.
There are two types of restless legs syndrome(3). Someone has primary restless legs syndrome if there is no known leading cause. Secondary restless legs syndrome, in contrast, stems from various identifiable causes.
This condition can be debilitating. Fortunately, it is now treatable thanks to medical advancements.
What Causes Restless Legs Syndrome?

Restless legs syndrome stems from a problem with dopamine systems and iron stores in the brain. Dopamine is the “happiness hormone.”
Certain genes may be tied to the development of RLS. Some patients have parents with the same condition.
However, there are many potential causes for secondary restless legs syndrome. Examples include:
- Varicose veins
- End-stage renal disease (ESRD)
- Celiac disease
- Fibromyalgia
- Amyloidosis
- Folate or magnesium deficiency
- Diabetes (Type 1 or Type 2)
- Iron deficiency
- Lumbosacral radiculopathy
- Rheumatic disease
- Certain depression medications
- Certain vitamin or mineral imbalances: lack of calcium, phosphate, vitamin D, and iron
Those with anemia, nerve problems, low ferritin, or high estrogen levels can develop restless legs syndrome. RLS is also common in pregnant patients, especially in the 3rd trimester(4).
Signs and Symptoms of Restless Legs Syndrome
RLS patients may describe a crawling, itching, or stretching feeling that seems to come from inside their muscles or bones. They might complain of paresthesia, or a prickling sensation, even when nothing touches their skin.
Patients experience involuntary and forceful backward foot bending that lasts 0.5-5 seconds. These movements can occur every 20 to 40 seconds during sleep and are experienced by most patients(1).
Symptoms can vary from mild annoyance to significant impairment, sometimes disrupting day-to-day life. Symptoms increase into the night, making it difficult for patients to sleep.
For patients with severe RLS, these movements occur whenever the patient sits.
Also, despite the name, RLS patients may sometimes experience arm and leg movements–not only legs.
Diagnosis of Restless Legs Syndrome
These symptoms are signs of restless legs syndrome… but they can also be signs of other ailments.
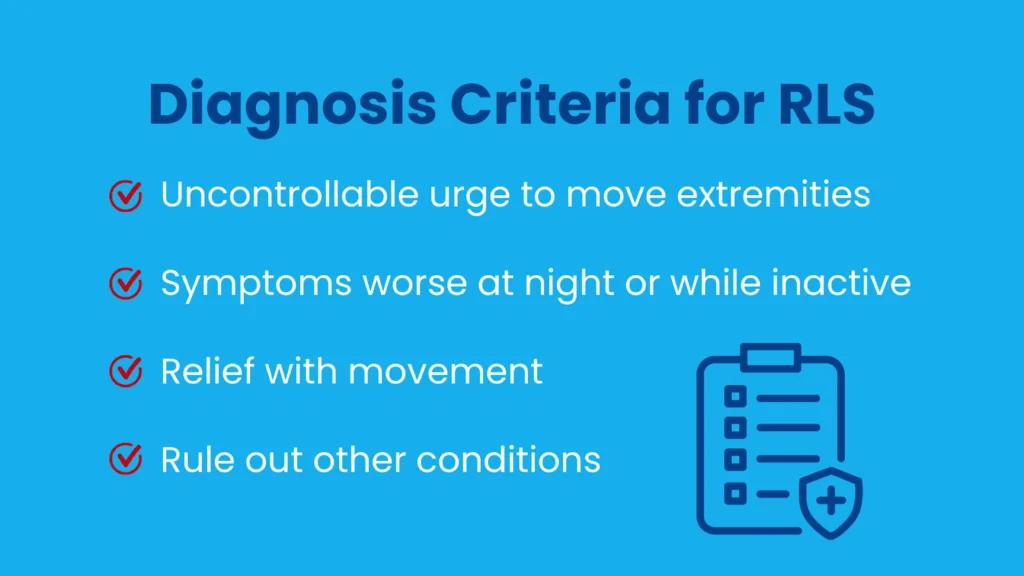
So how do you know if it’s RLS? You must meet this criteria(5).
- You feel an urge to move your leg or feet and uncomfortable sensations like paresthesia (that “crawling” or itching feeling).
- The urge to move these extremities worsens in the evening. The symptoms also appear while inactive.
- Leg movement may cause some or total relief. With continuous movement, the symptoms are often absent or mild.
- The urge to move the lower extremities is worst at night. This may make sleep difficult and cause fatigue the next day.
Finally, your doctor will rule out other conditions you may have, such as leg cramps, muscle cramps, and tardive dyskinesia. Symptoms must not also be from sitting in uncomfortable positions.
There is no specific test to diagnose restless legs syndrome. Medical professionals will perform other exams to test for related conditions. Your doctor may request an EMG, or electromyography, to rule out neuropathies or muscle disorders.
Treatments for Restless Legs Syndrome
To reduce restless legs syndrome symptoms, your doctor might recommend the following:
- Avoid or decrease caffeine intake.
- Avoid certain medications, such as antidepressants, antipsychotics, antiemetics, and centrally-acting antihistamines.
- Exercise daily(sometimes not recommended for patients who experience RLS while sleeping).
- Apply heat or a warm compress.
Medications such as pramipexole, ropinirole, rotigotine, and cabergoline may help decrease a patient’s symptoms. They can improve sleep and quality of life. Rotigotine transdermal patches can also be effective.
A doctor may prescribe gabapentin or pregabalin as early treatment for insomnia patients. It is also used for patients with pain, anxiety, and impulse control disorder.
These medications may have adverse effects or be harmful to certain patients. Consult with your doctor before starting any medications.
Radiofrequency ablation can help patients with secondary RLS and varicose veins. This is a minimally invasive varicose veins treatment. Treating the cause (varicose veins) can reduce secondary RLS symptoms.
Doctors may suggest dietary changes for those with specific vitamin or mineral deficiencies.
If a patient also suffers from renal failure, they may recommend short daily dialysis.
For pregnant women suffering from RLS, time is the best answer. Symptoms often improve after delivery.
Medication for Restless Legs Syndrome
Many medications can provide relief for restless legs syndrome patients. Medical professionals can provide recommendations based on a patient’s individual RLS experience.
One example is anti-seizure drugs: the FDA has approved gabapentin enacarbil for treating moderate to severe RLS. The drug has similar effects as dopaminergic treatment, another potentially helpful drug. Studies show pregabalin, another anti-seizure drug, is as effective for RLS as the dopaminergic drug pramipexole.
Dopaminergic agents are drugs that increase dopamine effects. They are prescribed to treat Parkinson’s disease. However, they can reduce the symptoms of RLS when taken at night.
The FDA has also approved ropinirole, pramipexole, and rotigotine to treat moderate to severe RLS. Side effects may include nausea, dizziness, and other short-term effects.
Long-term use of dopaminergic agents is not recommended as they can worsen symptoms. Stopping the medication can reverse the progression.
In extreme cases, doctors may prescribe certain opioids in low doses. Side effects can include constipation, dizziness, nausea, and risk of addiction.
Sometimes benzodiazepines are generally prescribed to treat anxiety, muscle spasms, and insomnia. Side effects may include daytime fatigue, reduced energy, and reduced concentration. (These are not recommended for sleep apnea patients.)
Share your symptoms and full medical history with your doctor. No two patients are exactly alike, and this will ensure you get the best treatment for your condition.
Conclusion
An estimated 7-10% of people suffer from restless legs syndrome. This condition is common! And 70% of these patients may have moderate to severe symptoms.
RLS is not always limited to legs. Some patients experience symptoms in their arms or hands.
When RLS impacts a patient’s sleep, they will experience fatigue during the day. Constant fatigue can lead to more severe complications, such as depression.
Restless legs syndrome can be more than an inconvenience. It can be debilitating and greatly impact the quality of life.
Fortunately, there are many ways to treat RLS and its symptoms. Understanding the ins and outs of RLS is the first step toward an improved quality of life.
References
- Mansur A, Castillo PR, Rocha Cabrero F, et al. Restless Leg Syndrome. [Updated 2020 Apr 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430878/
- Restless Legs Syndrome Fact Sheet. (n.d.). Retrieved from https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/restless-legs-syndrome-fact-sheet
- Pratt D. P. (2016). Restless Legs Syndrome/Willis-Ekbom Disease and Periodic Limb Movements: A Comprehensive Review of Epidemiology, Pathophysiology, Diagnosis and Treatment Considerations. Current rheumatology reviews, 12(2), 91–112. https://doi.org/10.2174/1573403×12666160223120340
- Prosperetti, C., & Manconi, M. (2015). Restless Legs Syndrome/Willis-Ekbom Disease and Pregnancy. Sleep medicine clinics, 10(3), 323–xiv. https://doi.org/10.1016/j.jsmc.2015.05.016
- Guo, S., Huang, J., Jiang, H., Han, C., Li, J., Xu, X., Zhang, G., Lin, Z., Xiong, N., & Wang, T. (2017). Restless Legs Syndrome: From Pathophysiology to Clinical Diagnosis and Management. Frontiers in aging neuroscience, 9, 171. https://doi.org/10.3389/fnagi.2017.00171




